Medicaid Reform
MAHP Supports Medicaid Reform to Fix Michigan’s Broken Mental Health System
Let’s fix the broken health care system and address the WHOLE person. Seven out of 10 adults with a behavioral health disorder reported having at least one physical disorder, according to national studies. That’s why MAHP supports Medicaid Reform legislation, SB 597 and 598, to make sure everyone gets the health care they need.
People with mental health concerns often have physical health issues. But today their care is not coordinated. We need one system that can help those with both conditions.
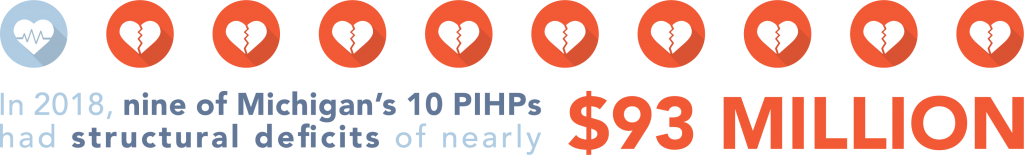
We aren’t just failing consumers. We are failing taxpayers. Nine out of Michigan’s 10 Prepaid Inpatient Health Plans (PIHPs) that oversee mental health treatment finances had structural deficits of nearly $93 million in 2018. Taxpayers deserve more accountability for the money spent.
Michigan needs a fully integrated physical and behavioral health system which will provide access to person-centered care, consumer choice, better transparency, ensure quality outcomes while continuing to be accountable stewards of Michigan taxpayers’ dollars. It will provide access to a contract-driven state system of managed whole person care, integrating behavioral health into the state’s successful physical health system that for more than 20 years has meant better care while controlling costs for the state’s Medicaid beneficiaries.
Michigan’s Medicaid health plans have a long history of streamlining the physical health needs of consumers in a cost-effective way, educating them about underlying physical conditions that may impact mental health and helping them address mental health needs in ways that will reduce physical health impacts.

Integration of behavioral health into primary care are intertwined because it:
- Treats the “whole person,” and recognizes mental and physical health conditions are often intertwined. For instance, chronic knee or back pain can lead to opioid addiction or as children age their social and emotional developmental issue can lead to physical ailments.
- Provides a comprehensive approach to care coordination across medical and behavioral services.
- Improves member and provider experiences.
- Reduces utilization and subsequent costs of costly services such as acute and emergency room admissions.
- Eases administrative complexity and reduces administrative costs.
- Increases capacity to deliver innovations within behavioral health.
Download Medicaid Reform resources and infographics
Medicaid Reform Myth vs. Fact
Read and download Medicaid Reform success stories
-
Coordination of All Physical Health & Behavioral Health Needs Through One Managed Care Organization
-
Medicaid Reform Success Stories, Part 1
-
Medicaid Reform Success Stories, Part 2
-
Medicaid Reform Success Stories, Part 3
-
Medicaid Reform Success Stories, Part 4
Download resources here for more information.
-
Integrating Behavioral Health into Medicaid Managed Care:
Design and Implementation Lessons from State Innovators
-
Exploring the Impact of Integrated Medicaid Managed Care on Practice-Level Integration of Physical and Behavioral Health
-
New Mexico Mental Health Epidemiology Fact Sheet Mental Health
